Gastrointestinal (GI) bleeding is a medical emergency that requires swift and comprehensive management. It occurs when there is bleeding in any part of the gastrointestinal tract, from the mouth to the rectum. Managing GI bleeds involves a series of steps, from diagnosis to treatment and recovery, to ensure the best possible outcome for the patient.
Diagnosis:
Diagnosing a GI bleed begins with a thorough medical history review and physical examination. Symptoms such as vomiting blood, passing dark stools (melena), or experiencing rectal bleeding prompt further investigation. Physicians might order various tests, including blood tests to check for anemia and determine the extent of blood loss, as well as endoscopic procedures like gastroscopy or colonoscopy to identify the bleeding site.
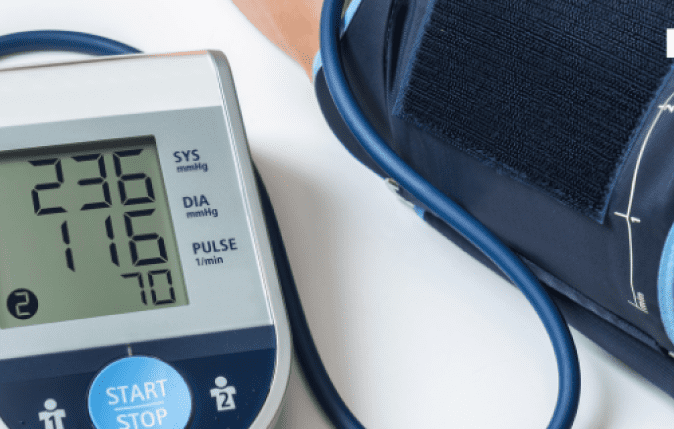
Stabilization:
Immediate stabilization is crucial to prevent further blood loss and stabilize the patient’s condition. Hemodynamic stability is assessed, and interventions may include intravenous fluids, blood transfusions to replace lost blood, and, in severe cases, medications or procedures to control bleeding.
Treatment:
Treatment options for GI bleeds depend on the cause and severity of the bleeding. Peptic ulcers, one of the common causes, might be treated with medications to reduce acid production or with endoscopic techniques like cauterization or clipping to stop bleeding. Vascular lesions might require embolization or angiographic intervention. In severe cases, surgery might be necessary to repair the bleeding source.
Recovery and Monitoring:
After the bleeding is controlled, the focus shifts to recovery and preventing future episodes. Close monitoring, especially in the initial 24-48 hours, is crucial to watch for re-bleeding or complications. Patients may need to follow dietary modifications and take medications to aid healing and prevent recurrence.
Post-Treatment Care:
Post-treatment care involves educating the patient about lifestyle changes, such as avoiding certain medications that can exacerbate bleeding, quitting smoking, and reducing alcohol consumption. Follow-up appointments with gastroenterologists or specialists help monitor the healing process and assess the effectiveness of the treatment.
Preventive Measures:
Prevention plays a pivotal role in managing GI bleeds. Identifying and addressing risk factors such as H. pylori infection, NSAID use, or underlying conditions like Crohn’s disease can help prevent recurrent bleeding episodes. Regular screenings and endoscopic surveillance in high-risk individuals contribute to early detection and intervention.
Collaborative Care:
Comprehensive GI bleed management often involves a multidisciplinary approach. Gastroenterologists, surgeons, hematologists, and other specialists collaborate to tailor treatment plans according to the individual patient’s needs. This collaborative effort ensures a holistic approach to care and improves patient outcomes.
Advancements in Technology:
Technological advancements have significantly impacted GI bleed management. Innovations in endoscopic devices, such as capsule endoscopy and advanced imaging techniques, aid in identifying bleeding sources more precisely and non-invasively. These technologies enhance diagnostic accuracy and treatment efficacy.
Conclusion:
Managing GI bleeds requires a systematic approach, from prompt diagnosis to stabilization, treatment, and subsequent recovery. A combination of medical interventions, lifestyle modifications, and preventive measures plays a pivotal role in successful management. Collaboration among healthcare professionals, coupled with advancements in technology, continues to improve outcomes for individuals experiencing GI bleeding.
By understanding the comprehensive approach to GI bleed management, healthcare providers can deliver more effective and tailored care, leading to better patient outcomes and improved quality of life for those affected by this condition.