Exploring the Benefits of Palliative Care
Palliative care is an important aspect of managing heart disease, especially in cases where curative treatment options are limited or the disease is advanced. It focuses on providing relief from symptoms, improving quality of life, and addressing the emotional and spiritual needs of patients and their families.
Here are some tips and tricks for palliative care in heart disease:
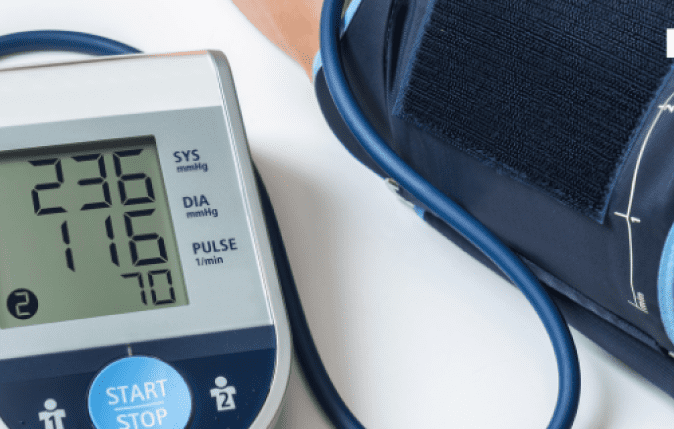
Symptom management : Palliative care focuses on managing symptoms to improve the patient’s comfort and quality of life. In heart disease, common symptoms include pain, shortness of breath, fatigue, and anxiety. Palliative care teams work closely with patients to identify the severity and impact of these symptoms. They may prescribe medications such as pain relievers or diuretics to reduce fluid retention and ease breathing. Additionally, they can teach patients breathing techniques, relaxation exercises, and energy conservation strategies to manage symptoms effectively.
Communication : Open and honest communication is vital in palliative care. Healthcare providers engage in discussions with patients and their families about the prognosis of the heart disease, available treatment options, and goals of care. These conversations help patients and their families make informed decisions based on their preferences and values. By discussing the benefits, risks, and potential outcomes of different treatment options, patients can understand the potential impact on their quality of life and choose the approach that aligns with their goals.
Emotional support : Dealing with heart disease can be emotionally challenging for patients and their loved ones. Palliative care teams provide emotional support through counseling, therapy, and support groups. They create a safe space for patients to express their fears, concerns, and emotions related to their illness. Emotional support also extends to family members who may be coping with stress, anxiety, or grief. By addressing emotional needs, palliative care promotes psychological well-being and helps patients and families navigate the emotional aspects of their journey.
Advance care planning : Advance care planning involves discussing and documenting a patient’s preferences for end-of-life care. Palliative care teams facilitate these conversations to ensure that patients’ wishes are respected and honored. This may include creating living wills, appointing healthcare proxies (someone who can make medical decisions on the patient’s behalf), and discussing resuscitation preferences. These discussions should be ongoing, regularly revisited, and updated as the patient’s condition changes.
Spiritual care : Palliative care recognizes the importance of addressing spiritual needs, which can vary among individuals. Healthcare providers may involve chaplains or spiritual counselors who can offer support and guidance. They respect and honor the patient’s religious or spiritual beliefs, and they may facilitate access to religious or spiritual practices that provide comfort. Spiritual care aims to provide solace, hope, and a sense of meaning during the challenging times associated with heart disease.
Support for caregivers : Caregivers play a vital role in supporting patients with heart disease. However, caregiving can be physically and emotionally demanding. Palliative care teams acknowledge and address the needs of caregivers by providing respite care, support groups, and counseling services. Respite care involves temporary relief from caregiving responsibilities to allow caregivers to take breaks, rest, and recharge. Support groups provide opportunities for caregivers to connect with others facing similar challenges, share experiences, and learn coping strategies. Counseling services can help caregivers navigate their emotions, manage stress, and develop self-care strategies.
Nutritional support : Nutrition plays a crucial role in managing heart disease. Palliative care teams provide dietary guidance tailored to the patient’s specific needs. They may recommend modifications to the patient’s diet to ensure they receive adequate nutrition while managing symptoms such as fluid retention or decreased appetite. Nutritional support aims to optimize the patient’s overall well-being, enhance energy levels, and minimize discomfort related to heart disease.
Enhancing quality of life : Palliative care aims to enhance the patient’s overall quality of life, regardless of the stage of heart disease. This involves a holistic approach that addresses physical, emotional, and psychosocial aspects. Palliative care teams assist patients with daily activities, facilitate social interactions, and encourage engagement in hobbies and interests. They provide resources and recommendations to improve comfort and well-being, such as assistive devices, relaxation techniques, and access to community support services. Enhancing the patient’s quality of life promotes a sense of dignity, autonomy, and fulfillment.
Multidisciplinary approach : Palliative care involves a multidisciplinary team consisting of healthcare professionals from various fields, including physicians, nurses, social workers, psychologists, and pharmacists. This collaborative approach ensures comprehensive care that addresses the complex needs of patients with heart disease. Each team member brings their expertise to provide holistic support, including symptom management, emotional support, advance care planning, spiritual care, and coordination of services. By working together, the team can optimize the patient’s care and well-being.
Continuity of care : Palliative care should be integrated into the patient’s overall care plan and provided throughout the disease trajectory. It involves ongoing coordination between the palliative care team and other healthcare providers involved in the patient’s care. This ensures a seamless transition of care as the patient’s condition changes or they move between different healthcare settings. Continuity of care promotes effective communication, shared decision-making, and consistent support for patients and their families.
It’s important to remember that palliative care in heart disease is personalized and should be tailored to meet the unique needs and goals of each patient. Healthcare professionals experienced in palliative care can provide individualized guidance and support based on the specific circumstances of the patient and their family.