Understanding the Risks of Eye Complications with Diabetes
Diabetes, a prevalent metabolic disorder, affects millions worldwide. While its impact on blood sugar levels is widely known, its ramifications extend to various organs, including the eyes. Understanding the specific risks and potential complications of diabetes-related eye issues is crucial for early detection and effective management. Let’s delve into the intricate relationship between diabetes and eye health to safeguard vision and overall well-being.
The Link Between Diabetes and Eye Health
Diabetes poses a significant risk to eye health due to its effect on blood vessels throughout the body, including those in the eyes. High blood sugar levels can lead to several complications, including:
- Diabetic Retinopathy: This condition affects the blood vessels in the retina, the light-sensitive tissue at the back of the eye. It is a leading cause of blindness among adults with diabetes.
- Diabetic Macular Edema (DME): DME occurs when fluid leaks into the macula, the central part of the retina responsible for sharp, central vision. It can lead to blurred or distorted vision and, if left untreated, permanent vision loss.
- Cataracts: People with diabetes are at a higher risk of developing cataracts, a clouding of the lens in the eye that can impair vision. Diabetes-related cataracts may develop at an earlier age and progress more rapidly than in individuals without diabetes.
- Glaucoma: Diabetes increases the risk of developing glaucoma, a group of eye conditions characterized by damage to the optic nerve. Glaucoma can lead to vision loss and blindness if left untreated.
Symptoms of Diabetic Eye Complications
In the early stages, diabetic eye complications may not cause noticeable symptoms. However, as the conditions progress, individuals may experience:
- Blurred or distorted vision
- Floaters or spots in the field of vision
- Fluctuations in vision
- Dark or empty areas in vision
- Difficulty seeing at night
- Eye pain or pressure
Prevention and Management Strategies
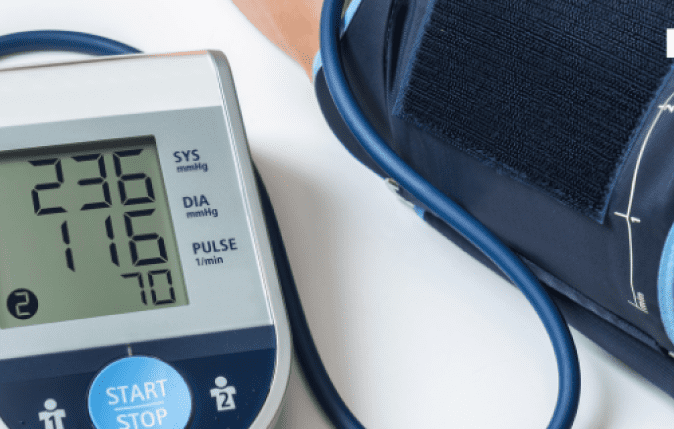
- Control Blood Sugar Levels: Maintaining stable blood sugar levels is crucial for preventing and managing diabetic eye complications. Follow your healthcare provider’s recommendations for diet, exercise, medication, and regular monitoring of blood glucose levels.
- Regular Eye Exams: Routine eye exams are essential for early detection of diabetic eye complications. Comprehensive dilated eye exams can detect signs of diabetic retinopathy, DME, and other eye conditions before they cause vision loss.
- Blood Pressure and Cholesterol Control: High blood pressure and cholesterol levels can exacerbate diabetic eye complications. Manage these risk factors through lifestyle modifications and, if necessary, medication prescribed by your healthcare provider.
- Healthy Lifestyle Habits: Maintain a healthy lifestyle by eating a balanced diet, engaging in regular physical activity, avoiding smoking, and managing stress. These lifestyle habits can help reduce the risk of diabetes-related eye issues and promote overall well-being.
Diabetes can have profound effects on eye health, increasing the risk of vision-threatening complications such as diabetic retinopathy, DME, cataracts, and glaucoma. However, with proactive management and regular eye care, the impact of diabetes on vision can be minimized. By controlling blood sugar levels, attending regular eye exams, and adopting healthy lifestyle habits, individuals with diabetes can protect their vision and enjoy a high quality of life for years to come. If you have diabetes, prioritize your eye health and work closely with your healthcare team to prevent and manage diabetic eye complications effectively.